- KYPROLIS® (carfilzomib) is indicated in combination with dexamethasone, or with lenalidomide plus dexamethasone, or with daratumumab plus dexamethasone, ... Read More Read Less
Flexible dosing options to meet the unique needs of your patients1
Phase 3, randomized, open-label, multicenter trial (n=478) comparing KYPROLIS® 70 mg/m2 once weekly plus dexamethasone to KYPROLIS® 27 mg/m2 twice weekly plus dexamethasone in patients with relapsed and refractory multiple myeloma who had received 2 to 3 prior lines of therapy. 78 patients were randomized 1:1 to receive KYPROLIS® 70 mg/m2 once weekly plus dexamethasone (n = 240) or KYPROLIS® 27 mg/m2 twice weekly plus dexamethasone (n = 238) for 28-day cycles until disease progression or unacceptable toxicity. The primary endpoint was PFS. Secondary endpoints included ORR and safety.2
Grade 3 adverse reactions of interest, Kd 70 mg/m2 once weekly (n=238) vs Kd 27 mg/m2 twice weekly (n=235): Peripheral neuropathy (0% vs 1%); acute renal failure (4% vs 6%); cardiac failure (3% vs 4%); ischemic heart disease (1% vs 1%); pulmonary hypertension (0% vs 1%).2
Kd = carfilzomib + dexamethasone; mg/m2 = milligrams per meter squared body surface area; PFS = progression-free survival; ORR = overall response rate.
*Until disease progression or unacceptable toxicity.
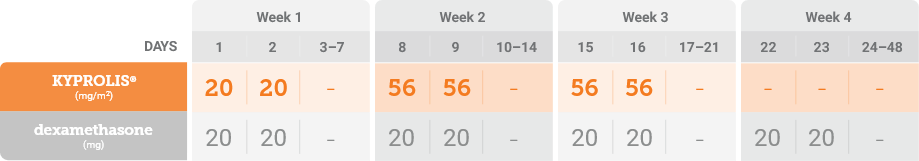
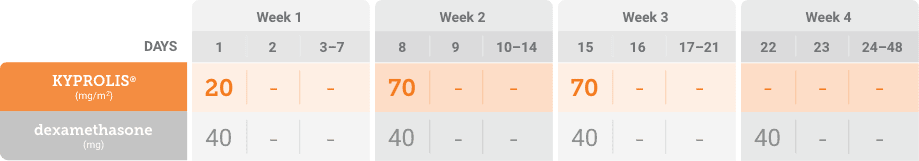
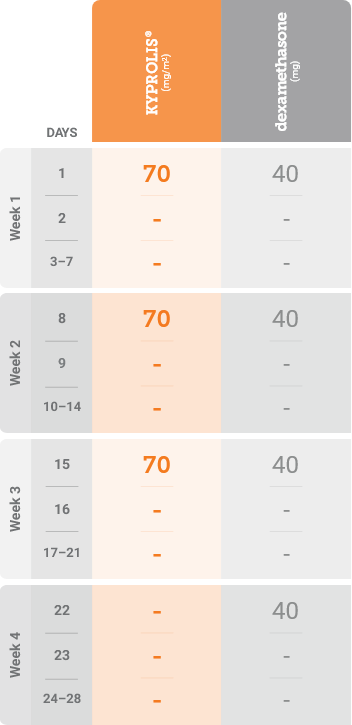
mg/m2 = milligrams per meter squared body surface area; mg = milligram.
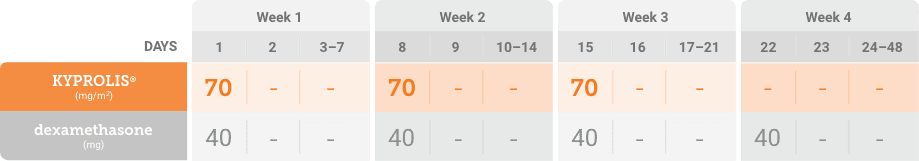
mg/m2 = milligrams per meter squared body surface area; mg = milligram.
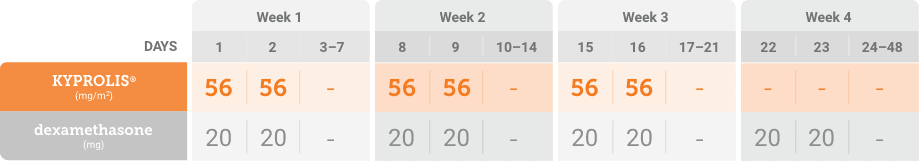
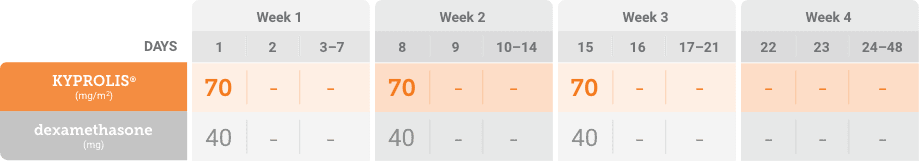
mg/m2 = milligrams per meter squared body surface area; mg = milligram.
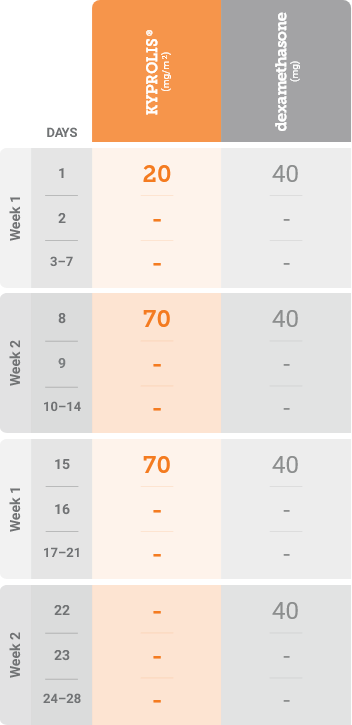
mg/m2 = milligrams per meter squared body surface area; mg = milligram.
Kd = carfilzomib + dexamethasone; mg/m2 = milligrams per meter squared body surface area; mg = milligram.
mg/m2 = milligrams per meter squared body surface area; mg = milligram.
mg/m2 = milligrams per meter squared body surface area; mg = milligram.
*Until disease progression or unacceptable toxicity.1
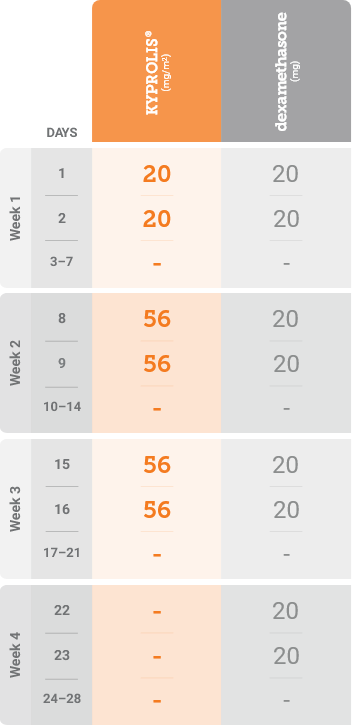
mg/m2 = milligrams per meter squared body surface area; mg = milligram.
mg/m2 = milligrams per meter squared body surface area; mg = milligram.
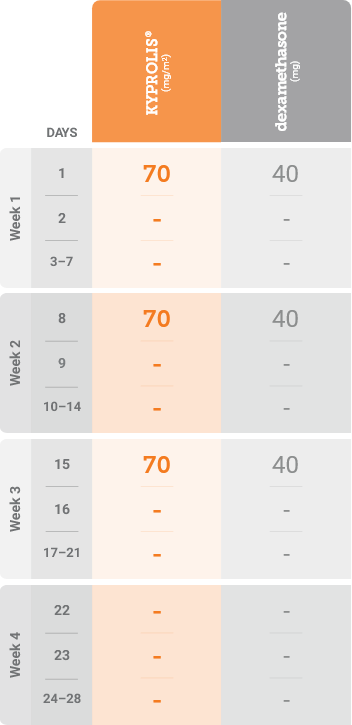
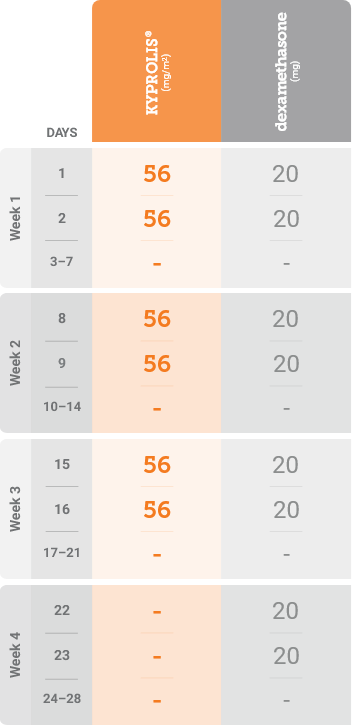
mg/m2 = milligrams per meter squared body surface area; mg = milligram.
Please see accompanying full Prescribing Information.
Please see accompanying full Prescribing Information.
References: 1. KYPROLIS® (carfilzomib) prescribing information, Onyx Pharmaceuticals Inc., an Amgen Inc. subsidiary. 2. Moreau P, Mateos M-V, Berenson JR, et al. Once weekly versus twice weekly carfilzomib dosing in patients with relapsed and refractory multiple myeloma (A.R.R.O.W.): interim analysis results of a randomized, phase 3 study. Lancet Oncol. 2018;19:953-964. 3. Mikhael J. Management of carfilzomib-associated cardiac adverse events. Clin Lymphoma Myeloma Leuk. 2016;16(5):241-245.